Top 10 Things to Know About Hydroxychloroquine
Hydroxychloroquine, also known as Plaquenil, is a medication used to treat malaria, lupus, and acute and chronic rheumatoid arthritis. Hydroxychloroquine has ... read more...also been mentioned as a possible COVID-19 treatment. While hydroxychloroquine has been used as an emergency treatment for certain COVID-19 patients, the FDA (Food and Drug Administration) recently revoked its Emergency Use Authorization. There is more information now about the safety and effectiveness of hydroxychloroquine as a COVID-19 treatment than there was at the start of the coronavirus outbreak. Learn about hydroxychloroquine's use in malaria treatment, why it's prescribed for lupus, and potential hydroxychloroquine side effects.
-
Hydroxychloroquine, which comes in tablet form, is categorized as a DMARD, or disease-modifying antirheumatic drug. Although the exact mechanism of action of the medication for treating autoimmune diseases like rheumatoid arthritis is unknown, it is believed to disrupt immune system cell communication.
DMARDS assist immune cells in staying focused on their original task rather than assisting a harmful disease or virus to take over. It has also been shown to reduce arthritis pain and swelling and may prevent joint damage.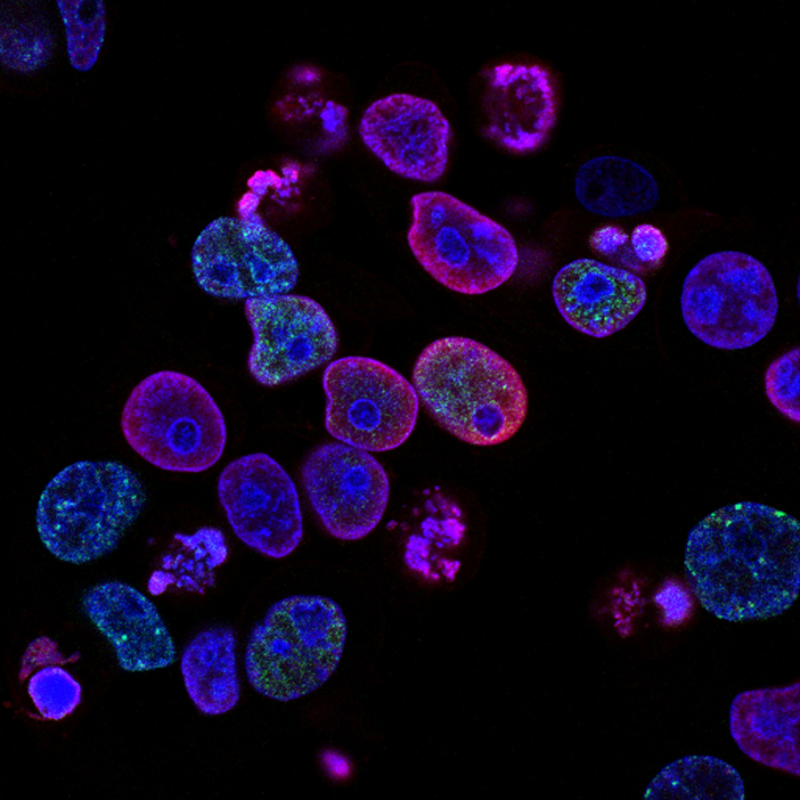
Photo by National Cancer Institute on Unsplash 
Image by Wälz from Pixabay -
Hydroxychloroquine, an antimalarial medication, is used to prevent malaria. You can obtain a prescription to take hydroxychloroquine before, during, and after a trip to a country where malaria is common. One dose per week will be administered beginning one week before the trip, one dose per week will be administered while on the trip, and one dose will be administered each week for four weeks after the trip.
The Centers for Disease Control and Prevention keeps an up-to-date list of places where this medication is advised for use; nonetheless, hydroxychloroquine is ineffective in all nations where malaria is common.
Image by 41330 from Pixabay 
Photo by CDC on Unsplash -
Antimalarial drugs were used to treat lupus as early as 1834. The FDA approved hydroxychloroquine as a treatment for both systemic lupus and rheumatoid arthritis in 1956.
It was shown to be effective in reducing the number of disease flares, reducing long-term damage, and delaying ultraviolet light absorption in lupus patients (photosensitivity is common among people with lupus).
In the case of rheumatoid arthritis, hydroxychloroquine can reduce pain and swelling, protect joints, and lower the risk of long-term disability.
Photo by Towfiqu barbhuiya on Unsplash 
Photo by Christina Victoria Craft on Unsplash -
Hydroxychloroquine, like most medications, can cause unwanted side effects.
With this drug, the most common side effects are stomach pain, nausea, vomiting, cramps, diarrhea, and headache.
Although itching, rash, changes in skin pigmentation, muscle weakness, and/or hair changes are uncommon, some patients do experience them.
Taking hydroxychloroquine with food can significantly reduce these side effects for many patients.
However, if patients experience more serious side effects such as low blood sugar, fainting, blurred vision, irregular heartbeats, or ringing in the ears, they should consult their doctors.

Photo by Kyle Glenn on Unsplash 
Image by Robin Higgins from Pixabay -
It's crucial for patients to discuss taking hydroxychloroquine with their doctor if they already have eye issues, particularly those involving the retina, because this medication has the potential to cause visual changes or loss of vision.
Before taking hydroxychloroquine, patients with diabetes, psoriasis, kidney disease, liver disease, blood or bone marrow problems, muscle problems, stomach or bowel problems, and/or nerve problems should consult with their doctor.
Furthermore, there is always the possibility of negative drug interactions, so it is critical to consult with your doctor to determine whether this drug will cause problems if combined with your current medications.
Photo by PhotoMIX Company: https://www.pexels.com/photo/person-holding-black-tube-1001897/ 
Photo by julien Tromeur on Unsplash -
Although there is no FDA-approved treatment for COVID-19, hydroxychloroquine was given to some patients who were hospitalized with the virus. The researchers discovered that hydroxychloroquine significantly shortened body temperature recovery time and cough remission time, as well as improved pneumonia, in a small study of 62 patients at the Renmin Hospital of Wuhan University in China.
Based on early promising results, the FDA granted Emergency Use Authorization (EUA) for hydroxychloroquine's use in certain COVID-19 patients who are not eligible for a clinical trial. However, the beneficial effect of hydroxychloroquine on COVID-19 recovery was not uniform. This fact, combined with the possibility of serious side effects, prompted the FDA to withdraw the EUA for hydroxychloroquine.
Patients with COVID-19 should not receive hydroxychloroquine treatment unless they are enrolled in a clinical trial for the drug.
Photo by Edward Jenner: https://www.pexels.com/photo/a-sick-man-covering-his-mouth-4031631/ 
Photo by Roman Grachev on Unsplash -
No one should use hydroxychloroquine to treat COVID-19 because it is still in the experimental stage and should only be used under a doctor's supervision.
In fact, hydroxychloroquine should not be obtained without a prescription. The CDC advises against purchasing this medication from a third party because the medications you receive may be of poor quality, contaminated, or counterfeit.
Furthermore, the National Capital Poison Center advises everyone to speak with a trusted healthcare provider or Poison Control to avoid misinformation that could lead to serious consequences, such as taking chloroquine in other, potentially fatal forms.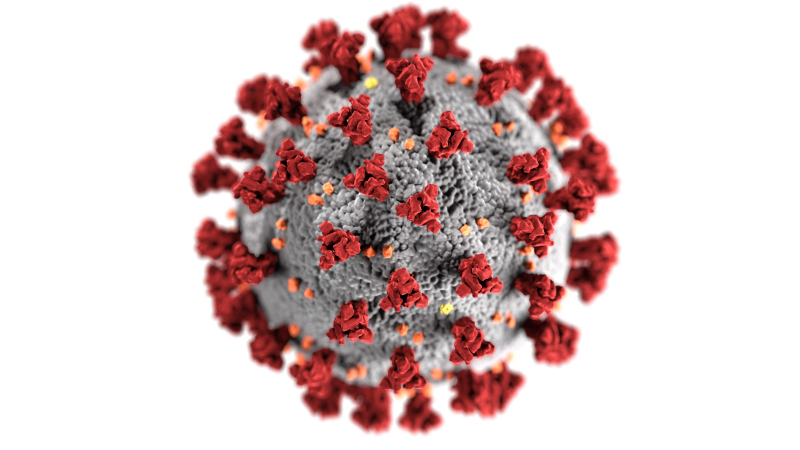
Photo by CDC on Unsplash 
Photo by Martin Sanchez on Unsplash -
Follow your doctor's instructions for using hydroxychloroquine exactly. Read all medication guides or instruction sheets and adhere to all instructions on your prescription label.
Unless your doctor instructs you otherwise, take hydroxychloroquine with food or a glass of milk.
A tablet of hydroxychloroquine shouldn't be broken or crushed.
Usually taken every day, hydroxychloroquine is used to treat lupus or arthritis.
Hydroxychloroquine is typically taken once per week on the same day each week to prevent malaria. Begin taking the medication two weeks before traveling to a region with a high malaria risk. Throughout your stay and for at least 4 weeks after you leave the area, continue taking the medication.
To treat malaria, hydroxychloroquine is usually administered in one large dose followed by smaller doses over the next two days.
Even if your symptoms improve quickly, continue to take this medication for the full duration prescribed.
If you have been exposed to malaria, or if you have fever or other symptoms of illness during or after a stay in an area where malaria is common, contact your doctor as soon as possible.
Protective clothing, insect repellents, and mosquito netting around your bed can help you avoid mosquito bites that can lead to malaria.
There is no medication that is completely effective in treating or preventing all types of malaria. Consult your doctor if you experience a fever, vomiting, or diarrhea during your treatment.You might require routine eye and medical tests while taking hydroxychloroquine.
Store away from moisture, heat, and light at room temperature.
Photo by National Cancer Institute on Unsplash 
Photo by Eiliv Aceron on Unsplash -
Get immediate medical help or dial 1-800-222-1222 for poison help. A hydroxychloroquine overdose needs to be treated right away because it can be fatal.
Drowsiness, altered vision, seizures, a weak pulse, pounding heartbeats, sudden dizziness, fainting, shortness of breath, or slow breathing are just a few of the overdose symptoms that can occur (breathing may stop).
Keep hydroxychloroquine away from young people. A child who unintentionally takes too much hydroxychloroquine could die.

Image by Jan Alexander from Pixabay 
Photo by Engin Akyurt: https://www.pexels.com/photo/woman-in-blue-and-white-face-mask-4056211/ -
Your heart may be adversely affected by hydroxychloroquine, particularly if you also take certain other medications, such as the antibiotic azithromycin (Z-Pak). If you experience sudden dizziness and a racing or pounding heartbeat, call for emergency medical help (like you might pass out).
Long-term or high-dose use of hydroxychloroquine may permanently harm the retina of your eye, leading to vision problems that cannot be reversed.
If you experience blurred vision, difficulty focusing, distorted vision, blind spots, difficulty reading, changes in your color vision, or increased sensitivity to light, stop taking hydroxychloroquine and contact your doctor right away.
Photo by DS stories: https://www.pexels.com/photo/photograph-of-a-lit-red-heart-candle-9228393/ 
Photo by Ksenia Chernaya: https://www.pexels.com/photo/woman-examining-eyesight-in-medical-clinic-5752271/












