Top 10 Common Misconceptions About Schizophrenia
Schizophrenia is a form of psychotic condition distinguished by hallucinations, delusions, and a distorted perception of reality. Disordered cognitive ... read more...processes, disorganized speech, aberrant movement, and social isolation are other prominent signs of schizophrenia. One of the most misunderstood mental health problems is schizophrenia. Learn more about schizophrenia and the truth of these common misconceptions about it.
-
This is incorrect. Schizophrenia frequently causes a range of symptoms, but none of them include multiple personalities. The majority of the population's only encounter with the condition is through movies or media. As a result, they are unable to detect the signs of schizophrenia. Believing incorrectly that patients with the condition have "split" or multiple personalities. The term "schizo" literally means "split" in Greek. However, it refers to gaps (or a splitting) in a person's ability to think and express emotions in this scenario. Split personalities, also known as Dissociative Identity Disorder or Multiple Personality Disorder, are not the same as schizophrenia.
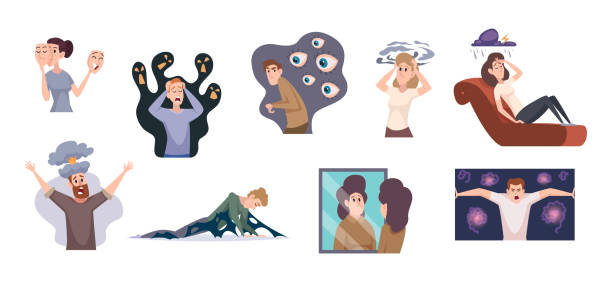
For persons suffering with schizo, there is a divide between reality and fantasy. Delusions and hallucinations may occur, and emotions may become inappropriate. There is uncertainty regarding who is genuine and who is not. Many people mistakenly assume that patients with schizophrenia only have hallucinations and delusions. This comes as no surprise. Psychotic symptoms are distinctive and frequently terrifying. As a result, popular culture emphasizes these symptoms more than other symptoms linked with schizophrenia. Schizophrenics are known to hear voices and see things that are not real. However, they can have negative symptoms such as poor motivation and trouble developing social bonds. They are dissatisfied with their daily routines. According to the American Psychological Association, they seldom talk and have difficulties paying attention.

istockphoto 
istockphoto -
Stable people can perform pretty well when they remain on top of their medication and use psychosocial therapy. According to the National Alliance on Mental Illness, up to half of the two million Americans living with schizophrenia can considerably improve. If they receive therapy, they may even recover entirely. Working can genuinely aid in the recovery of those suffering from schizophrenia. It can be used for vocational rehabilitation.
Independence and empowerment can be beneficial components of the healing process. However, it is psychosocial support that makes true healing feasible. Psychotherapy, family education, and self-help groups can assist persons suffering with schizophrenia in coping and regaining control of their life. Treatments such as social skills therapy, job training, and vocational counseling can also be beneficial. Applying for disability benefits is another option.

istockphoto 
istockphoto -
Not all people suffering from schizophrenia require long-term hospitalization. Some persons with this disorder live with family members or in group homes. If a person has schizophrenia symptoms for the first time, or if they continue to have schizophrenia symptoms despite therapy and medication, they may be hospitalized. Since the 1990s, there has been a steady growth in the number of publications and research on schizophrenia.
Some typical schizophrenia treatment modalities include:
- Therapeutic methods that block dopamine receptors in the brain (e.g., antipsychotic medications)
- Behavioral and psychotherapy, with the overall goal to address cognitive impairments and improve memory
- Improving psychosocial interactions (e.g., workplace rehabilitation)
The length of a person's treatment will be determined by how they respond to treatment techniques. The Mayo Clinic states that schizophrenia symptoms require lifetime treatment, however long-term institutionalization may not be required unless symptoms are severe.

istockphoto 
istockphoto -
Despite the fact that the vast majority of people with schizophrenia are not violent, a sizable section of the society perceives them to be such, owing to media representations of the condition. The great majority of films involving people with schizophrenia presented them as murderous maniacs or conducting violent crimes, according to the researchers. People with schizophrenia, however, are more likely to be injured by others than to harm themselves due to the disorder's stigma.
Although some research has found that individuals with schizophrenia are four to seven times more likely to commit violent crimes than the general population, many studies have shown that the risk arises in patients with confounding variables associated with violence, such as substance abuse, which exist regardless of the presence of schizophrenia.
According to a 2012 survey, the majority (80%) of films with schizophrenia characters presented these people as aggressive. Although this study only looked at films made between 1990 and 2010, it is possible that more current films with schizophrenic characters will be more responsive to genuine schizophrenia facts. Another 2016 study discovered that several films exaggerated the characters' schizophrenia symptoms for dramatic purposes. This exaggeration is most likely the result of a total misunderstanding of the disorder, which is inconsiderate to individuals who suffer from it.

istockphoto 
istockphoto -
Schizophrenia manifests itself differently in each individual and comprises a wide range of symptoms. Auditory hallucinations and other sorts of sensory illusions, such as hearing voices, are common in certain persons. A common media cliché is that a person with schizophrenia hears a scary voice in their brain encouraging them to do violent acts. According to study, people's interpretations of auditory hallucinations may be impacted by their culture. Although patients with schizophrenia in the United States were more likely to describe nasty and threatening voices, people with schizophrenia in India and Ghana had mostly good encounters with their voices.
One explanation for the disparity might be sociocultural factors. Voices were perceived as invasive to one's private life in individualist countries such as the United States, but individuals in collectivist societies stressing community felt more comfortable forming relationships with their voices.

istockphoto 
istockphoto -
Schizophrenia is caused by distinct genetic and environmental risk factors and is not caused directly by poor parenting. It is a prevalent misconception that poor parenting or tough relationships cause schizophrenia. This stereotype could possibly be falser. There are various genetic origins of schizophrenia. Each of them has a minor influence on the overall progression of the illness. Severe childhood stress or trauma, as well as infections that activate the immune system, are all risk factors for developing schizophrenia.
A minor loss on chromosome 22 is another genetic risk factor. All of a person's genetic information is stored on chromosomes. A minor loss on chromosome 22 can predispose a person to not just schizophrenia but also cardiac, immunological, and developmental disorders (cleft palate). There may be certain environmental and psychological elements that contribute to the development of schizophrenia, but they must be objectively proven.

istockphoto 
istockphoto -
Believe it or not, there are a variety of apparently unrelated variables linked to the development of schizophrenia. Growing up in a city is related with a twofold increase in the chance of getting schizophrenia. Furthermore, the age of one's father during conception is associated to the likelihood of acquiring the disease. Intriguingly, the season of one's birth may also influence the risk of schizophrenia: people born in late winter and early spring are more likely to acquire the condition than the rest of the population.
While none of the causative processes have been proven, a few ideas exist to explain each. Psychologists have hypothesized that variables such as pollution and increased exposure to social stress may contribute to the link between schizophrenia and urbanization. Furthermore, researchers have theorized that so-called de novo mutations, modifications in spermatogonial stem cell divisions that occur more frequently with age, are responsible for the increased risk of mental illnesses, including schizophrenia, in late fatherhood. Finally, studies have indicated that moms who get a virus while pregnant have children who are more likely to develop schizophrenia.
Although further study is needed, psychologists believe that the increased prevalence of schizophrenia in children born in late winter and early spring may be due to the close proximity to the flu season a few months earlier. The combination of these and other factors implies that the causation of schizophrenia is complicated and will require more research to completely understand.
istockphoto 
istockphoto -
Schizophrenia has no effect on a person's IQ. High intellect is frequently associated with schizophrenia in the popular media. In 2014, research was done to investigate this potential link. The study found no link between genius or high IQ and the development of schizophrenia.
Another study discovered that persons who acquire schizophrenia perform worse on IQ tests both before and after the start of the illness. There have also been stories of people with extremely high IQs developing schizophrenia. Nonetheless, these people account for a relatively tiny number of instances.

istockphoto 
istockphoto -
Schizophrenia is connected to bipolar illness and schizoaffective disorder, both of which are characterized by mood swings that are abrupt and alternating. However, schizophrenia is a very different disorder. Another myth about schizophrenia is that people have unexpected mood swings, which is not true. Bipolar disorder is a condition in which a person's moods cannot be controlled. Mood swings can vary from depressed to happy to manic. Likewise, schizoaffective disorder has all of the symptoms of schizophrenia as well as a mood condition such as bipolar disease.
As a result, someone who displays signs of schizophrenia as well as mood swings most likely has schizoaffective disorder rather than schizophrenia. Mood stabilizers and antidepressants are commonly used to treat bipolar illness, whereas antipsychotic medication is used to treat schizophrenia. A combination of antipsychotics and antidepressants or mood stabilizers may be prescribed in the case of schizoaffective disorder.

istockphoto 
istockphoto -
Several evidence-based therapies are available for schizophrenia. There are now numerous emphases on the treatment of schizophrenia. Along with antipsychotic drugs that target dopamine receptors in the brain, emerging pharmacologic treatments target glutamate, glycine, and acetylcholine receptors.
Other schizophrenia therapies include:
- Cognitive-behavioral treatment (CBT)
- Transcranial magnetic stimulation (TMS)
- Deep neural stimulation
- An integrated approach to the health treatment of schizophrenia patients (mind and body)
istockphoto 
istockphoto