Populations at increased risk
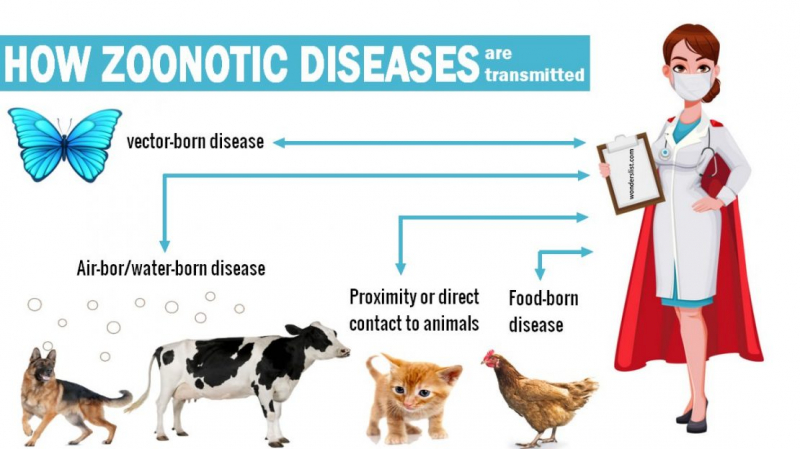
A zoonotic illness can infect anybody who comes into touch with an affected animal, vector, or polluted place. However, the risk of disease, clinical indications of disease, and mortality are not distributed evenly across people. Certain risk variables influence the proportion of patients who remain asymptomatic and the case fatality rate (the proportion of sick people who die). Age, for example, is frequently linked to illness severity. Very young children and the elderly are more prone than older children and healthy adults to develop potentially deadly hemolytic uremic syndrome (HUS) if they become infected with Escherichia coli O157:H7 by contact with animals or their surroundings.
Hantavirus, on the other hand, appears to be more lethal in fit young adults and middle-aged people, probably due to the higher risk of such people coming into touch with the infectious agent. Immunosuppression from a previous disease or medicine increases the chance of being infected with a zoonotic disease. Cryptosporidiosis, for example, caused by Cryptosporidium parvum and transmitted to people by contact with calves, their dung, or manure-contaminated items or food, can arise as a coinfection with acquired immunodeficiency syndrome (AIDS). Normally a self-limiting condition, cryptosporidiosis in AIDS patients can cause significant sickness, occasionally leading to death.
People who do not have a functional spleen are at a higher risk of disease and death from Capnocytophaga canimorsus infection, which can be contracted through contact with cats or dogs (particularly through dog bites). People who take chloroquine for malaria prophylaxis alongside rabies preexposure vaccines are less likely to build a strong enough immune response to survive a rabies infection.