Top 7 Things to Know About Clonidine
Clonidine (also known as Catapres) is an antihypertensive drug, used to treat high blood pressure and prevent strokes, heart attacks, and kidney problems. To ... read more...learn more about this drug, read our article.
-
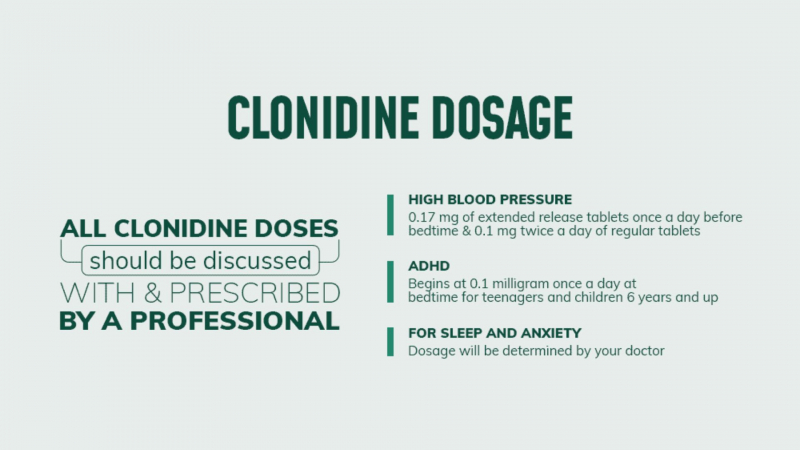
Clonidine can be used to treat high blood pressure as well as other conditions like attention deficit hyperactivity disorder (ADHD).
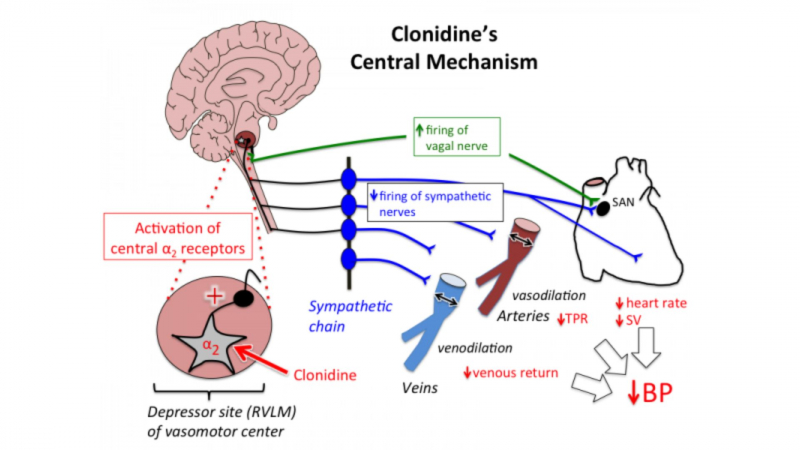
Clonidine reduces heart rate and blood pressure by acting on alpha-adrenoreceptors in the brain stem.
Clonidine's mode of action in ADHD is unknown.
Clonidine is a member of the drug class known as centrally acting alpha agonists.
TMedWeb 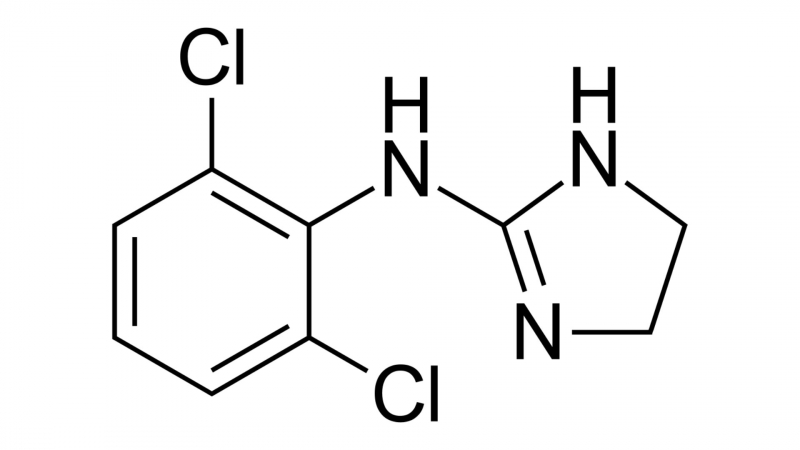
Wikipedia -
Clonidine may be used to treat high blood pressure when all other treatments have failed. It is usually used in conjunction with other medications to treat high blood pressure.
Slow-release formulations (Kapvay brand) may be used to treat ADHD (Attention Deficit Hyperactivity Disorder) in children over the age of six.
Off-label use for other conditions such as Tourette's syndrome is also possible (off-label means not an FDA-approved use but experts consider it still has a place in therapy).
There are three formulations available: an oral tablet, a transdermal patch, and an oral extended-release tablet. The transdermal patch may have fewer side effects than the oral form of the drug, but people who use it should be monitored for the appearance of a rash.
Clonidine is available in generic form.
Northpoint Seattle 
Northpoint Seattle -
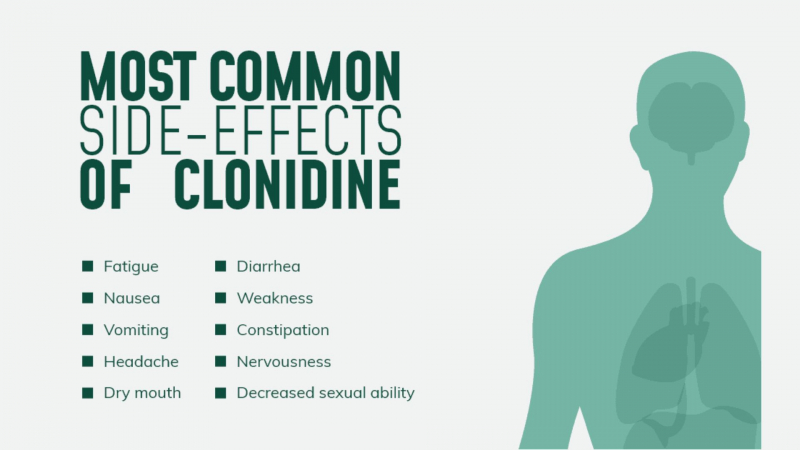
If you are between the ages of 18 and 60, do not take any other medications, and have no other medical conditions, you are more likely to experience the following side effects:
- Dry mouth, drowsiness, headache, fatigue, dizziness when standing, dry eyes, and constipation are some of the symptoms. Clonidine may lower blood pressure and increase the risk of falling when transferring from a lying or sitting position to a standing position. Clonidine drowsiness can impair a person's ability to drive or operate machinery.
- Agitation, anxiety, hallucinations, skin reactions, slow heart rate, and increased sensitivity to alcohol are some of the less common side effects. The use of clonidine has been linked to skin rash.
- Withdrawal symptoms include anxiety, agitation, tremor, and headache, as well as a rapid rise in blood pressure; taper off slowly on the advice of a doctor, and reinstate clonidine if necessary.
- Transdermal clonidine may cause an initially localized skin rash at the site of application; continued use may result in a more generalized rash; seek immediate medical attention.
- Clonidine may aggravate or cause arrhythmias, especially when combined with other medications that affect the sympathetic nervous system (such as epinephrine).
- Some people, including those who have previously experienced allergic reactions to clonidine, may be ineligible.
- When using for children, use caution, especially if they have a gastrointestinal illness that may cause vomiting and insufficient tablet absorption.
- Can be given up to 4 hours before surgery and then resumed shortly after.
- For the elderly, a dosage reduction may be necessary.
- Clonidine should be used during pregnancy only if the advantages outweigh the risks. Clonidine is excreted in breast milk, so use caution when administering it to a lactating woman.
Seniors and children, people with certain medical conditions (such as liver or kidney problems, heart disease, diabetes, seizures), or people who take other medications are more likely to experience a broader range of side effects.
Northpoint Seattle 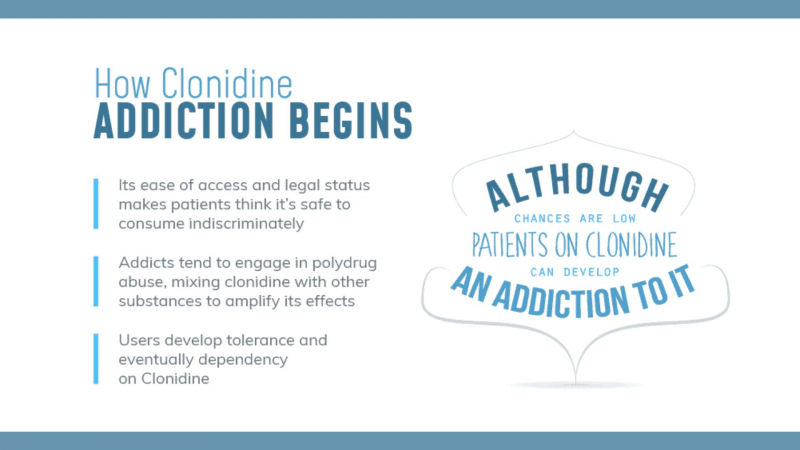
Northpoint Recovery -
Avoid driving or operating machinery until you know how clonidine affects your functioning.
Clonidine formulations are not interchangeable; consult your pharmacist.
Slow-release clonidine should not be crushed or chewed; instead, it should be swallowed whole.
Clonidine absorption is unaffected by food.
Do not stop taking without consulting your doctor; a slow withdrawal period of at least 2 to 4 days may be required.
Blood pressure and kidney function may need to be checked on a regular basis.
Clonidine-induced dry eyes may impair contact lens wear; use lubricant eye drops or seek medical advice.
Taking the majority of your clonidine dose at night may help reduce the occurrence of daytime sedation and dry mouth.
If you miss a dose, take it as soon as possible; do not take more than the prescribed amount in a 24-hour period.
Traffic desk 
Orlando Pharmacy -
Clonidine is quickly absorbed, with peak effects occurring within one to three hours. Clonidine's blood pressure-lowering effect occurs quickly, within 30 to 60 minutes of an oral dose, and the maximum effect occurs within two to four hours.
It may be used in conjunction with other ADHD medications. Clonidine-induced improvement in ADHD symptoms may take several days to manifest.

Cleveland Clinic Health Essentials 
AiHealth -
Medicines that interact with clonidine may reduce its effect, shorten its duration of action, increase side effects, or have no effect when combined. An interaction between two medications does not always necessitate the discontinuation of one of them; however, it can. Consult your doctor about how to handle drug interactions.
Clonidine may interact with the following medications:
- alpha-blockers such as prazosin or terazosin
- amphetamines which may diminish the blood pressure-lowering effects of clonidine
- antidepressants, such as fluoxetine, paroxetine, St John’s Wort, monoamine oxidase inhibitors, and tricyclic antidepressants (such as amitriptyline, imipramine, and nortriptyline)
- beta-blockers such as atenolol or metoprolol
- calcium channel blockers, such as diltiazem or verapamil
- cyclosporine
- digoxin
- duloxetine
- levodopa
- methylphenidate
- opioids, such as oxycodone or morphine
- some medications used to treat mental illness, such as clozapine or thioridazine
- zolpidem.
Clonidine may interact with other heart-rate-regulating medications.
It should be noted that this list is not exhaustive and only includes common medications that may interact with clonidine. For a complete list of interactions with clonidine, consult the prescribing information.
Vinmec 
Vinmec