Top 10 Most Expensive Medical Procedures
Medicine is one of the world's largest markets. People want to be healthy and recover from chronic diseases. Modern medicine allows for this, but at a high ... read more...cost. It includes cutting-edge research and technology, as well as the education and experience of doctors. The most expensive procedures are surgical interventions. Their cost is determined not only by the complexity of the procedure, the equipment used, and so on, but also by preliminary training, postoperative rehabilitation, maintenance personnel work, and so on. Today, Toplist is discussing the most expensive medical procedures in the world.
-
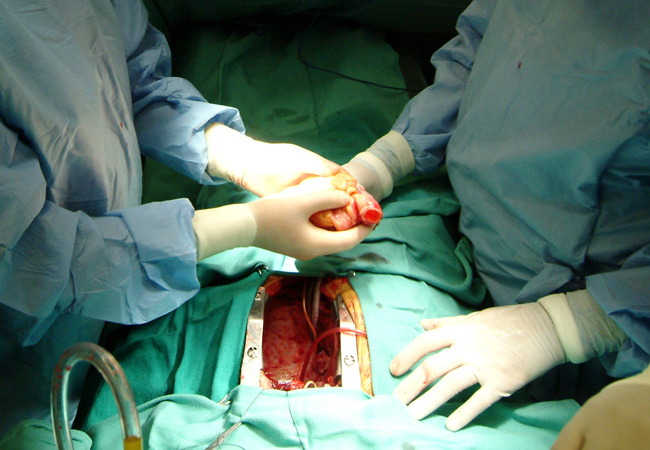
A heart transplant is a surgical procedure that involves removing a person's diseased heart and replacing it with a healthy heart from an organ donor. At least two healthcare providers must declare the organ donor brain dead.
When medications, lifestyle changes, and other treatment options fail and the patient is at the end stage of heart failure and the only option left is a heart transplant, only this surgical procedure is performed. To be eligible for a heart transplant, the individual must meet certain criteria.
Every year, approximately 3500 - 5000 heart transplants are performed worldwide; however, more than 50,000 candidates require transplantation. Due to the scarcity of organs, heart transplant surgeons and other healthcare providers must carefully consider who should receive a heart transplant.
There are numerous factors that can influence costs:
- Choosing a Doctor and a Hospital Location
- The cost of hospital and room.
- The surgeon's abilities and experience.
- The cost of diagnostic tests.
- Hospitalization.
- Insurance coverage can have an impact on a person's out-of-pocket expenses.
Cost: $1.4 million
consultqd.clevelandclinic.org Video: Perioperative Interactive Education's Youtube Channel -
Some people are unaware that lung transplants are possible. Lung transplantation is a surgical procedure that involves removing an unhealthy lung and replacing it with a healthy lung from a donor. The price rises because the lungs are a vital and very delicate organ. Furthermore, the patient requires a machine that will "breathe" for him or her during the operation. Of course, the price includes the lungs themselves, the work of specialists, life support equipment, medications to prevent the lung from being rejected by the body, and so on.
A lung transplant can be performed for a variety of reasons, including respiratory diseases, lung collapse, or even when breathing stops. People who have exhausted all other options for treating lung problems seek lung transplants. Damaged lungs are unable to deliver oxygenated blood to body parts. As a result, lung transplantation is required. People with chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, cystic fibrosis, and high blood pressure in the lungs are common candidates for lung transplantation.
Certain patients may require the replacement of both lungs (Double Lung Transplant). This is especially true for people with cystic fibrosis, because bacteria commonly colonize the lungs of such patients; if only one lung is transplanted, bacteria in the native lung could potentially infect the newly transplanted organ.
Cost: 1.2 million

spectrumnews1.com 
wexnermedical.osu.edu -
Intestine transplantation (also known as intestinal transplantation or small bowel transplantation) is one of the most expensive medical procedures that replaces the small intestine in both chronic and acute cases of intestinal failure. While alternative therapies such as parenteral nutrition (PN) can often treat intestinal failure, complications such as PN-associated liver disease and short bowel syndrome may make transplantation the only viable option. Intestine transplantation, one of the most uncommon types of organ transplantation, is becoming more common as a therapeutic option due to advancements in immunosuppressive regimens, surgical techniques, PN, and clinical management of pre and post-transplant patients.
There are three types of intestine transplants: isolated intestinal grafts, combined intestinal-liver grafts, and multivisceral grafts that include other abdominal organs. Only sections of the jejunum and ileum are transplanted in the most basic and common graft, an isolated intestinal graft. These procedures are carried out in the absence of liver failure. In the event of severe liver dysfunction caused by PN, enzyme deficiencies, or other underlying factors, the liver and intestine may be transplanted together. The stomach, duodenum, pancreas, and/or colon may be included in a multivisceral graft. When the underlying condition significantly compromises other sections of the digestive system, such as intra-abdominal tumors that have not yet metastasized, extensive venous thrombosis or arterial ischemia of the mesentery, and motility syndromes, multivisceral grafts are considered.
Intestinal transplants are sometimes combined with liver transplants, which raises the cost to around $1,121,800. Almost 80% of these costs are for hospital administration and recovery.
Cost: about $1.1 million

e.vnexpress.net 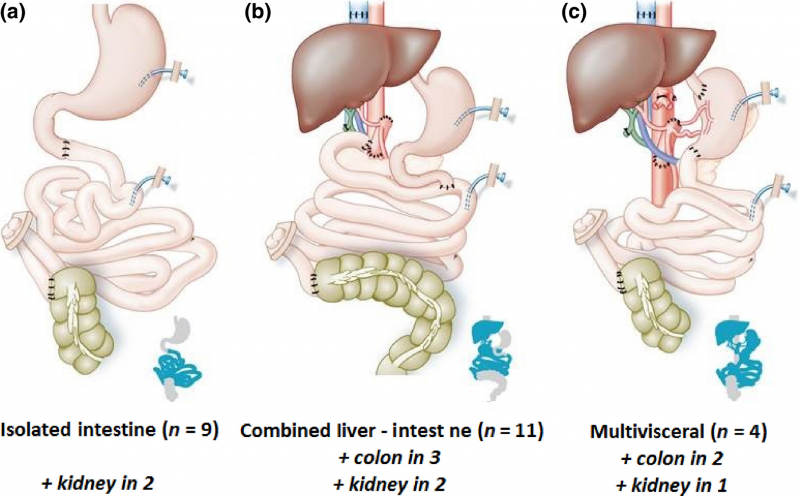
onlinelibrary.wiley.com -
Bone marrow is composed of soft tissue, blood vessels, and capillaries and is found in the center of many bones. The primary function of bone marrow is to produce blood cells that aid in the maintenance of a healthy vascular and lymphatic system, with over 200 billion cells produced each day. Both red and white blood cells are produced by the bone marrow. The constant production and regeneration of these cells is critical in aiding the body's fight against disease and infection, as well as in keeping the respiratory system operational.
A variety of medical conditions, including leukemias and cancers, tuberculosis, and sickle cell anemia, can impair bone marrow production. Diseases affecting the bone marrow can be fatal if left untreated. The first step in treating a bone marrow disease is the surgical removal of the affected bone marrow. This is analyzed to provide a diagnosis and to determine which treatment option is best. If cancerous cells are found, the most likely treatment will be chemotherapy or radiotherapy, with the goal of destroying the cancer cells and preventing them from spreading further. A number of red and white blood cells will be damaged as well. A bone marrow transplant is the most effective way to treat a bone marrow condition because it replaces damaged marrow and cells with new, healthy ones. Stem cells, which are early development cells capable of producing both red and white blood cells, are typically used in bone marrow transplants.
The stem cells are injected from donor blood marrow, which can come from an external donor or from within the patient. External donor stem cells must be a very close match to the patient's and are typically taken from the pelvic area. The donor stem cells are infused into the patient's bone via a vein using a drip infusion, which is a painless and minimally invasive procedure. Over the course of several hours, the donor material travels to the bone marrow. It will take 2 to 4 weeks for the implanted stem cells to begin producing new red and white blood cells, and the patient will need to remain isolated during this time due to the high risk of infection.
An allogeneic bone marrow transplant is a complex procedure that necessitates the expertise of experienced specialists and can thus be costly. Many people choose to seek treatment in another country, either to save money or to find specialized care.
Cost: $890,000

moffitt.org 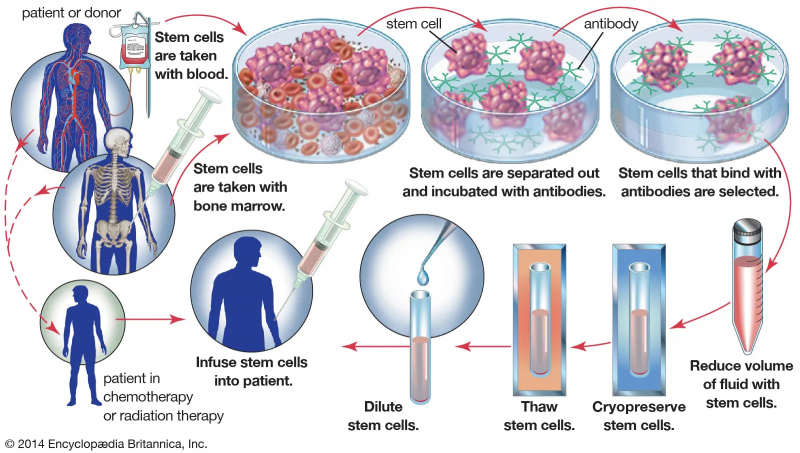
britannica.com -
Toplist would like to continue the list of the most expensive medical procedures by introducing you to a single lung transplant. A single lung transplant is a surgical procedure in which one lung is replaced with a donor lung. A donor lung can be obtained from either a living or deceased donor. A living donor can only donate one lobe of the lung. With some lung diseases, a recipient may only require a single lung transplant. Other lung diseases, such as cystic fibrosis, require that a recipient receive two lungs, so the Double Lung Transplant procedure is used. While lung transplants have some risks, they can also increase life expectancy and improve the quality of life for people with end-stage pulmonary disease.
Many patients can benefit from a single healthy lung transplant. The donated lung is usually from a donor who has been declared brain-dead. The average hospital stay after a lung transplant is one to three weeks, though complications may necessitate a longer stay. Following this stage, patients are usually required to attend a rehabilitation gym for 3 months to regain fitness. The rehabilitation program includes light weights, an exercise bike, a treadmill, stretches, and other activities.
Cost: $850,000
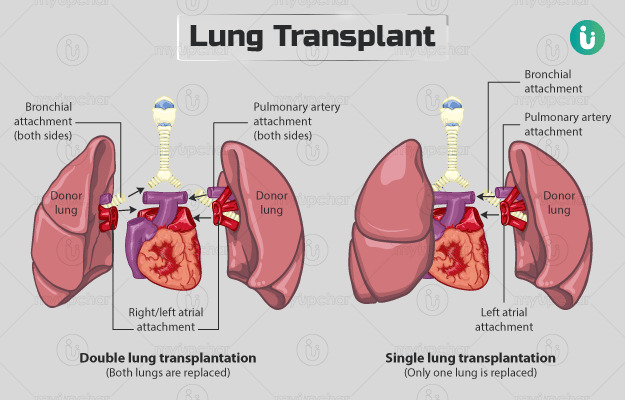
The differences between double and single lung transplant (myupchar.com) Video: Perioperative Interactive Education's Youtube Channel -
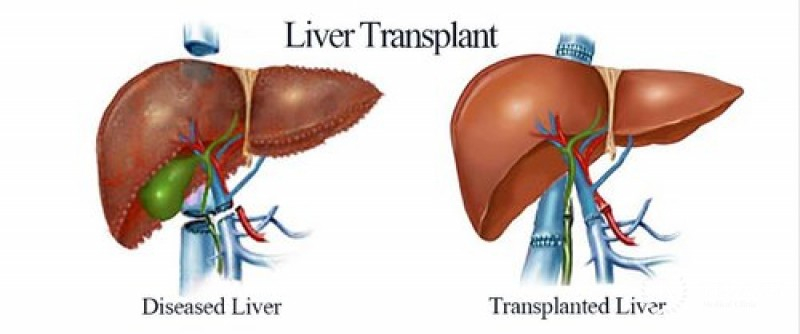
The replacement of a diseased liver with a healthy liver from another person is known as liver transplantation or hepatic transplantation (allograft). Although donor organ availability is a major limitation, liver transplantation is a treatment option for end-stage liver disease and acute liver failure. The most common technique is orthotopic transplantation, which involves removing the native liver and replacing it with the donor organ in the same anatomic position as the original liver.
The surgical procedure is complicated, requiring meticulous harvesting of the donor organ and implantation into the recipient. Liver transplantation is strictly regulated and is only performed at designated transplant medical centers by highly trained transplant physicians and their support teams. Depending on the outcome, the surgery can last anywhere from 4 to 18 hours. A well-calibrated live or cadaveric donor match, as well as careful screening for eligible recipients, are required for favorable outcomes.
Liver transplantation may be used to treat acute or chronic conditions that result in irreversible and severe ("end-stage") liver dysfunction. Because the procedure carries relatively high risks, is resource-intensive, and necessitates major life changes following surgery, it is reserved for emergency situations. Because outcomes are highly variable, judging the appropriateness/effectiveness of liver transplantation on a case-by-case basis is critical.
Cost: $812,500
tamc.co.il 
uwhealth.org -
To continue, Toplist would like to introduce to you Autologous Bone Marrow Transplant. In the case of autologous BMT, ex vivo procedures such as cytotoxic drug treatment, exposure to monoclonal antibodies that attack tumor-associated antigens, or harvesting and introducing stem cells (cells from peripheral blood) are used to destroy the malignant cells in the patient's marrow prior to reinfusion.
In the treatment of severe lupus, autologous bone marrow transplantation (ABMT) has been tried. In 2011, an international evaluation of ABMT in more than 200 adult patients with refractory disease revealed a 50% to 70% remission rate at 5 years, but a significant early mortality rate must be addressed through improved patient selection, induction, maintenance, and long-term patient follow-up. There have been reports of allogenic bone marrow transplantation and allogenic bone marrow mesenchymal stem cell transplantation being successful in adult SLE patients. Today, Autologous Bone Marrow Transplant is among the most expensive medical procedures at $410,000.
Cost: $410,000

bioinformant.com 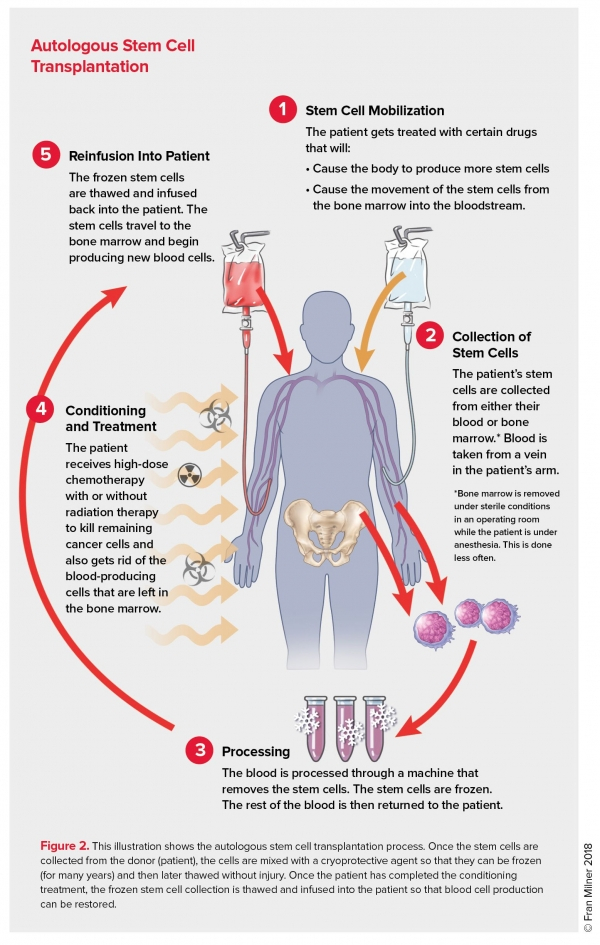
lls.org -
A kidney transplant is a surgical procedure that involves the placement of a healthy kidney from a living or deceased donor into a person whose kidneys are no longer functioning properly. The kidneys are two bean-shaped organs located just below the rib cage on each side of the spine. Each one is roughly the size of a fist. Their primary function is to produce urine, which filters and removes waste, minerals, and fluid from the blood.
When your kidneys lose their ability to filter, harmful levels of fluid and waste accumulate in your body, raising your blood pressure and leading to kidney failure (end-stage kidney disease). The end-stage renal disease occurs when the kidneys have lost approximately 90% of their normal function.
End-stage kidney disease is caused by a variety of factors, including:
- Diabetes
- Chronic, uncontrolled high blood pressure
- Chronic glomerulonephritis — an inflammation and eventual scarring of the tiny filters within your kidneys (glomeruli)
- Polycystic kidney disease
To survive, people with end-stage renal disease must have waste removed from their bloodstream using a machine (dialysis) or a kidney transplant.
A kidney transplant is a surgery that replaces a kidney (or both) from a living or deceased donor in a patient suffering from chronic renal disease. The kidneys are a natural filter in the human body that removes waste substances from the blood. When they lose this ability due to some pathologies, it indicates that the patient is suffering from kidney failure.
Dialysis or a kidney transplant are the only two options for treating kidney failure or end-stage kidney disease. Because it is possible to live with only one kidney, one healthy kidney will be sufficient to replace both failed kidneys and ensure the patient's healthy recovery. The transplanted kidney could come from either a living or a deceased donor. Patients with kidney failure or end-stage kidney disease should take this medication. It is among the most expensive medical procedures at $400,000.
Cost: $400,000
thelancet.com 
nbcnews.com -
A pancreas transplant is an organ transplant in which a healthy pancreas (one that can produce insulin) is implanted into a diabetic person. The recipient's native pancreas is left in place, and the donated pancreas is attached in a different location because the pancreas is a vital organ that performs functions necessary in the digestion process. In the event of the new pancreas being rejected, which would quickly lead to life-threatening diabetes, there is a good chance the recipient would not survive very long without the native pancreas, however dysfunctional, still in place. The healthy pancreas comes from a recently deceased donor, or it could be a portion of a pancreas from a living donor.
Pancreas transplants are currently performed on people with insulin-dependent diabetes, which can lead to serious complications. Patients with the most common and lethal form of pancreatic cancer (pancreatic adenomas, which are usually malignant and have a poor prognosis and a high risk of metastasis, as opposed to more treatable pancreatic neuroendocrine tumors or pancreatic insulinomas) are usually ineligible for valuable pancreatic transplants, because the condition has a very high mortality rate and the disease, which is usually highly malignant and detected too late to treat, to reduce surgical complications with enteric or bladder drainage, a better surgical method can be chosen. Immunosuppression progress has improved quality of life after transplantation.
Pancreas transplantation is typically performed on people with type 1 diabetes who have end-stage renal disease, brittle diabetes, and hypoglycemic unawareness. However, certain type 2 diabetics may benefit from a pancreas transplant as well. A type 2 diabetic has a BMI < 30 kg/m2 and a low overall insulin requirement (1 U/kg/day). The vast majority of pancreas transplants (> 90%) are simultaneous pancreas-kidney transplants.
Cost: $350,000

hospitalpharmacyeurope.com 
healthline.com -
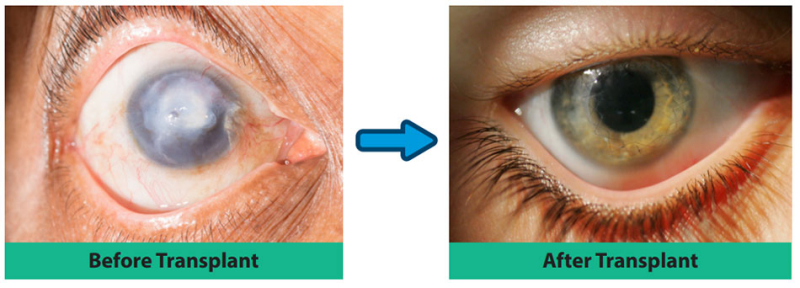
The cornea is the clear part of the eye that protects the iris, pupil, and anterior chamber. It is in charge of refracting light so that we can see. The cornea is composed of five distinct layers, each of which serves a distinct function, such as absorbing nutrients and oxygen from tears and preventing foreign objects from entering the eye. It thus protects the eye from damage caused by minor abrasions. Deeper abrasions can cause scarring in the cornea, reducing its transparency. When the cornea is damaged, the eye can no longer refract or bend light, causing difficulty seeing.
Cornea Transplantation may be performed to treat the damaged cornea and restore vision. Cornea transplantation is a surgical procedure in which the surgeon removes diseased or damaged corneal tissue and replaces it with healthy tissue. Deceased human donors provide healthy corneal tissue. The transplant can restore clear vision, allowing the patient to live a better life.
A corneal transplant can also be used to treat ulcers, complications from previous eye surgery, swelling or clouding of the cornea, and bulging out of the cornea. It is critical to locate a donor cornea prior to the procedure. Finding a donor cornea is no longer a difficult task because many people expressly request that their corneas be donated after death. However, corneas cannot be donated by deceased patients who had nervous system conditions, infections, or prior eye surgery or problems.
A Cornea Transplant is a complex procedure that requires the expertise of experienced specialists and can thus be costly. Cornea Transplant in India, Cornea Transplant in Turkey, and Cornea Transplant in Thailand are all options. Please contact us for more information.
Cost: $30,000
fvhospital.com 
https://www.westoncontactlens.com/